Doctors may soon have a new tool in the fight against one of the most aggressive and lethal forms of cancer—in the form of an ‘early warning’ signature of precancerous cells.
This is the promise of a new study by researchers at the University of California San Diego, who have found a link between inflammation, cellular stress and pancreatic ductal adenocarcinoma (PDAC), the most common type of pancreatic cancer.
PDAC, which develops from cells that lines small ducts in the pancreas, leaves patients with an average 5-year survival rate of less than 10 percent. In 2023, it was estimated that the disease manifested in more than 62,000 new cases in the U.S. alone.
Pancreatic cancer generally can only be controlled if it is found before it has spread, at which point it can be removed by surgery. If it has spread, palliative treatment can help to manage symptoms and complications of the disease to improve a patient’s quality of life.
The findings of the new study could help increase the rate at which PDAC is caught early enough to prevent it becoming life-threatening.
Previous studies have shown that inflammation and cellular stress activate a protein called “signal transducer and activator of transcription 3” (STAT3 for short) in pancreas cells.
STAT3 promotes the genesis of tumors, their adaptation to stress—which allows them to survive and spread—and their resistance to treatment. How it did this had long been unclear.
In their new study, however, the researchers report that in some cancer cells, STAT3 activates specific genes that play a critical role in adapting to inflammation and stress.
“Given the fact that STAT3 plays such an important role in many cancers and the fact that it controls so many genes prompted us to drill down on which genes in particular are associated with cancer development, progression and drug resistance,”paper author and pathologist David Cheresh told .
Specifically, they found that—in the presence of inflammatory proteins and stress induced by low oxygen levels—the protein turns on a gene called “Integrin β3” (ITGB3) in both mouse and human pancreas cells. ITGB3 then promotes the formation of PDAC tumors and accelerates the cancer’s progression.
Similarly, the team found that the inflammation and cellular stress caused by chemotherapy also activates STAT3, increasing ITGB3 expression in pancreatic cells.
In what could offer fresh hope for PDAC patients, the researchers found that blocking the protein’s inflammatory pathway can help delay tumor formation.
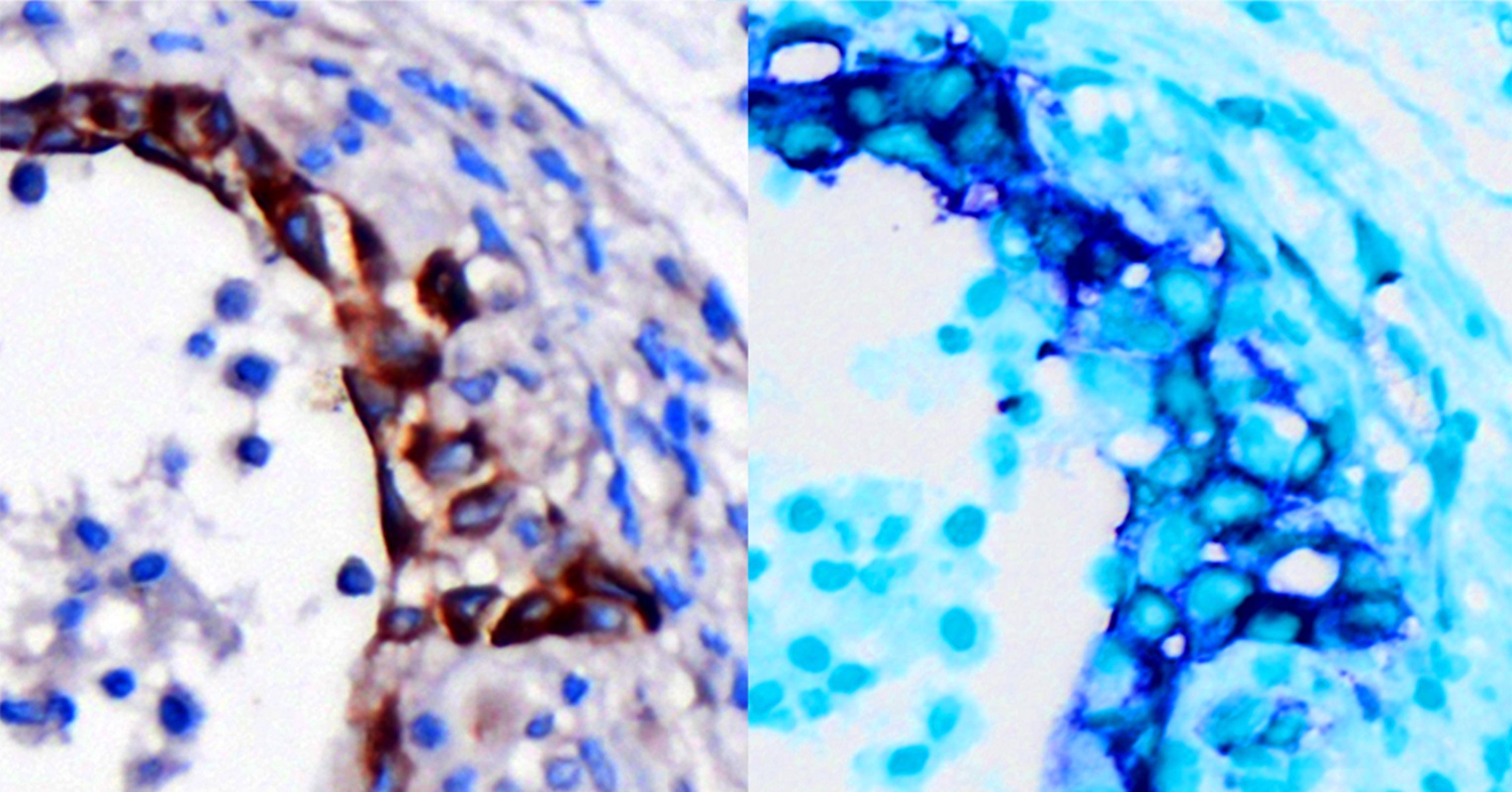
According to the researchers, STAT3 induces the expression of 10 genes in total— including ITGB3—that together form a prognostic gene signature the researchers have appropriately dubbed “STRESS UP”.
“A significant number of patients are what we refer to as ‘inducible’ for these STRESS UP genes including ITGB3,” said Cheresh.
Not only can the detection of the STRESS UP signal predict whether precancerous cells would develop into full-blown pancreatic cancer, but it can also be used to assess how aggressive a tumor is likely to become.
Having knowledge of this gene signature in patients could be valuable since there are known drugs on the market for other diseases that block STAT3 activation and thereby inhibit the expression of the STRESS UP genes in cancer cells,” Cheresh added.
“We observed that the STRESS UP gene signature is linked to various critical stages of cancer development including: tumor initiation as precancerous lesions develop into actual tumors, as tumors develop drug resistance and as tumors develop an invasive or metastatic behavior [when cancer spreads].”
Given this, the researchers believe that STRESS UP could be used to help develop early screening tools for PDAC, helping doctors to identify which patients are more likely to develop aggressive cancers and which will respond better to traditional pancreatic treatment at later stages.
We are now examining each of these STRESS UP genes for their specific role in the development and progression of cancer with the hope that new specific therapies can be developed. We already have one such therapeutic just now entering clinical trials for patients with drug resistant cancers,” said Cheresh.
Looking ahead, the team are starting to explore molecules that could stop inflammation from activating ITGB3 in not only pancreatic cancer, but also other cancers that affect the surface of tissues— including lung, breast and skin cancers.
This could help prevent tumors from progressing, spreading and becoming resistant to drug therapies, they said.
has reached out to the researchers for comment.
Do you have a tip on a health story that should be covering? Do you have a question about pancreatic cancer? Let us know via health@.
Update 07/23/25, 07:28 a.m. ET: This article was updated with additional information and comments from David Cheresh.
Reference
Campos, A. D., Shepard, R. M., Ortega, Z., Heumann, I., Wilke, A. E., Nam, A., Cable, C., Kouhmareh, K., Klemke, R., Mattson, N. M., Ideker, T., De Arruda Saldanha, C., Heinz, S., Weaver, V., Von Schalscha, T., Wettersten, H. I., Weis, S. M., & Cheresh, D. A. (2025). A STAT3/integrin axis accelerates pancreatic cancer initiation and progression. Cell Reports, 116. https://doi.org/10.1016/j.celrep.2025.116010
Related Articles

